Abstract
The optimal regimen intensity before allogeneic hematopoietic cell transplantation (HCT) remains an unsettled question. The recent Blood and Marrow Transplant Clinical Trial Network BMTCTN 0901 randomized phase III study showed that Myeloablative conditioning (MA) results in better relapse-free survival and a trend towards better overall survival compared to reduced intensity conditioning (RIC). The findings of BMTCTN 0901 though contradicts several prior studies addressing the same question, was limited by the fact that most patients in the RIC received fludarabine/low dose Busulfan and the study was not designed to assess the effect of intensity on patients with different disease risk index (DRI) groups. Acute myeloid leukemia and myelodysplastic syndrome patients with low/intermediate DRI tend to respond well to chemotherapy and can potentially be cured with chemotherapy regimens alone. On the other hand, high and very high risk DRI myeloid malignancies have a high relapse rate and very low rates of success with chemotherapy only approach. We hypothesize that conditioning intensity benefit is limited to patients with low/intermediate risk DRI and no such benefit is seen in the high/very high risk DRI myeloid malignancy patients. To answer this question, we retrospectively analyzed AML/MDS HCT recipients with low/intermediate DRI to assess the impact of conditioning intensity on overall survival (OS), disease free survival (DFS), relapse, and non-relapse mortality (NRM). Survival was calculated using the Kaplan-Meier estimator. Univariate analysis with Gray test and log-rank test will be used for cumulative incidence and survival respectively. Cox regression models were built to study the effect of conditioning intensity adjusted for other significant factors on OS, NRM, DFS, relapse and graft-versus-host disease (GVHD). Conditioning intensity was retained in the cox models and other variables were selected to be included if the P-value was less than 0.05.
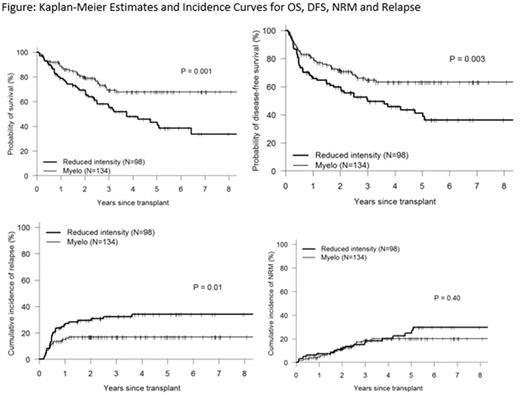
A total of 232 consecutive allogeneic HCT recipients with low/intermediate DRI myeloid malignancy (AML 170, MDS 60) were included in the analysis with a median follow up of 37 months. Median age was 55 years (18, 75) and 83% were of white race. Patient and transplant related characteristics were as follows: 42% RIC, 11% Myeloablative high dose TBI, 47% non-TBI Myeloablative conditioning; 21% bone marrow graft; 31% matched related donor transplant MRDT, 47% matched unrelated donor transplant MUDT, 22% haploidentical donor HIDT; 49% had hematopoietic cell transplant comorbidity index HCT-CI ≥3 ; donor/recipient female to male 21%; and donor/recipient CMV +/+ 42%, -/- 19%, other 39%. Both MA and RIC groups had similar patient, disease and transplant related characteristics except for a higher percentage of MA recipients received methotrexate as part of their GVHD prophylaxis compared to RIC (78% vs 55%, p<0.001). Recipients of Myeloablative conditioning had better overall survival estimate (3-year 69% vs 57%, p=0.001), DFS (3-year 65% vs 51%, p=0.003) and lower relapse cumulative incidence (3-year 17% vs 32%, p=0.01) but similar NRM (3-year 19% vs 17%, p=0.04) to RIC recipients (figure 1). There was no difference in the cumulative incidence of grade 2-4 acute and moderate-severe GVHD between Myeloablative and RIC groups. Multivariate analysis revealed MA conditioning to be associated with better DFS (HR 0.58, 95% CI 0.39-0.88, p=0.01), lower relapse (HR 0.56, 95% CI 0.32-0.97, p=0.038) and similar NRM (HR1.11, 95% CI 0.54-2.26, p=0.781) compared to RIC. When same analysis was performed for high/very high DRI myeloid malignancy patients (N=247), conditioning intensity had no effect on OS, DFS, Relapse and NRM (P value>0.10 for all).
Myeloablative conditioning results in better overall survival and disease control when compared to RIC among AML/MDS patients with low/intermediate DRI risk group. This benefit is not shown among high/very high DRI risk patients.
Solh: Celgene: Speakers Bureau; ADC Therapeutics: Research Funding; Amgen: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal